Abstract
Introduction:
Controversy exists regarding whether high-intensity (such as 7+3) versus low-intensity (such as hypomethylating agent or low-dose cytarabine) therapy represents an optimal therapy for older patients with AML. While some retrospective studies have demonstrated an overall survival advantage with high-intensity therapy, others including a prospective study (Blood. 2015;126:291-299) failed to confirm these results. Although somewhat arbitrary, several factors influence patients' and physicians' choices of therapy selection. In this context, we performed a single-center retrospective study at the University of Nebraska Medical Center to determine treatment practices in older patients with AML.
Methods:
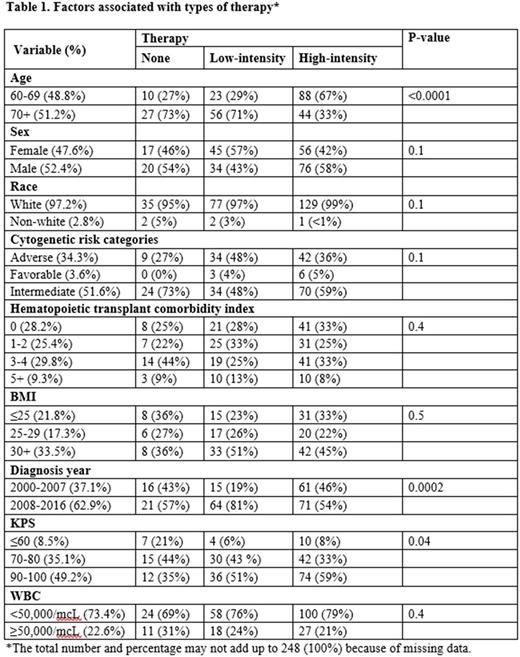
We utilized the institutional cancer registry and electronic medical records to extract patient-level data of 248 older patients (aged 60 years or older) diagnosed with AML between the years 2000-2016. Only analytic cases (patients initially diagnosed and/or treated at our institution) were included. Data abstracted include age, gender, race, hematopoietic transplant comorbidity index (HCT CI), body mass index (BMI), year of diagnosis, Karnofsky performance status (KPS), white blood cell (WBC) count, cytogenetic risk categories and type of therapy (none, high- and low-intensity therapy). Fisher's exact test, and logistic regression (for multivariate analysis) were used to determine an association between the type of therapy and other characteristics.
Results:
Patient characteristics and univariate analysis are provided in table 1. Patients had a median age of 70 years, adverse cytogenetics in 38%, and a median BMI of 28. Median total bilirubin and creatinine were 0.6 mg/dL (range 0.1-2.8) and 1.0 mg/dL (range 0.5-5.5) respectively. 30% had HCT CI score of 0, 27% score of 1-2, 32% score of 3-4, and 10% score of 5+. Patients had KPS of ≤60 (8%), 70-80 (35%), 90-100 (49%). Median number of medications at diagnosis included 6 (range 0-27). Receipt of therapy included none (15%), low-intensity (32%) and high-intensity (53%). 15% of all patients underwent allogeneic HCT. Patients aged 60-69 years were more likely to receive high-intensity therapy. The use of low-intensity therapy such as hypomethylating agents was higher, and fewer patients received no therapy in the years 2008-2016. The use of high-intensity therapy was higher with higher KPS. In a multivariate analysis, only age and time period were significantly associated with the use of low versus high-intensity of therapy. The odds of getting low-intensity therapy for patients aged 70+ years was 7.3 (95% CI: 3.6-15.1) times higher than that for patients aged 60-69 years.
Conclusion:
Our unselected cohort study provides data regarding comorbidities, BMI and medication use at baseline in older patients. The study demonstrates variations in the treatment practices in older patients, particularly based on age. The use of low-intensity therapy has increased in more recent years. Patients' preferences and physicians' judgment of anticipated therapy tolerance were not captured in this retrospective study and likely accounts for much variation in therapy use. Such unmeasured selection bias may also preclude accurate comparison of the results across trials or across two arms in non-randomized trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal